Background
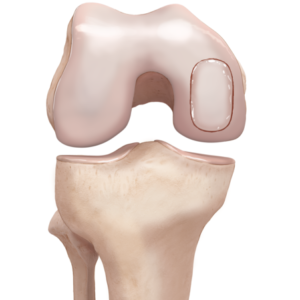
There are 2 main cartilage structures in the knee. The hyaline cartilage, also called articular cartilage, lines the end of the bone surfaces of the femur, tibia and patella (the kneecap), acting as a smooth, gliding surface permitting knee joint movement.
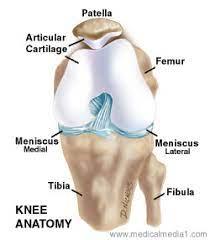
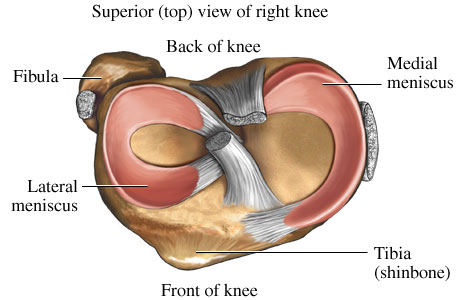
The meniscus, a second type of cartilage, acts as a shock absorber in the knee, preventing damage to the articular cartilage.
When articular cartilage is damaged, it often causes symptoms such as pain, swelling and locking in the knee. The cartilage relies on the surrounding joint fluid for its nutrition and has a poor blood supply, hence its inability to regenerate or heal on its own. If left untreated, damaged cartilage predisposes the knee to early arthritis.

Most of the time, damaged articular cartilage requires surgery to remove the non-healing tissue and then an additional procedure to restore or help to regenerate cartilage.
These procedures are described below:
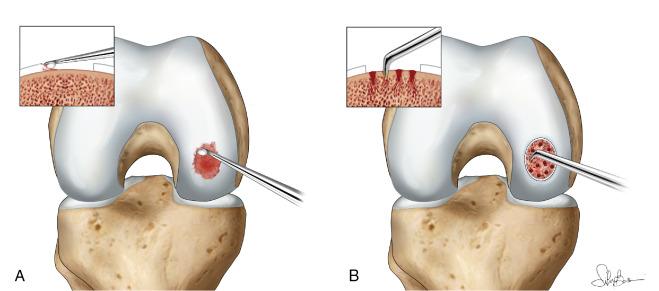
1 - Microfracture- this arthroscopic or ‘keyhole’ procedure involves making small perforations in the subchondral plate to cause bleeding and stem cells to migrate into the cartilage defect. ‘Scar’-cartilage or fibrocartilage is formed. This is not as robust as the native ‘hyaline’ cartilage
2 - Cartilage transplantation- cartilage can be harvested from the patient’s own knee in non-essential areas or can be obtained from a donor. There are pros and cons to each strategy. Harvesting one’s own cartilage can lead to ‘donor-site’ issues and is limited by the amount of non-essential cartilage available. For larger areas of damage, donor cartilage can be used to fill the defect. The donor cartilage is placed into the knee through an open procedure where the damaged tissue is removed and the donor cartilage is implanted. Donor cartilage carries the risk of allergic reaction, graft rejection by one’s own immune cells and infection.
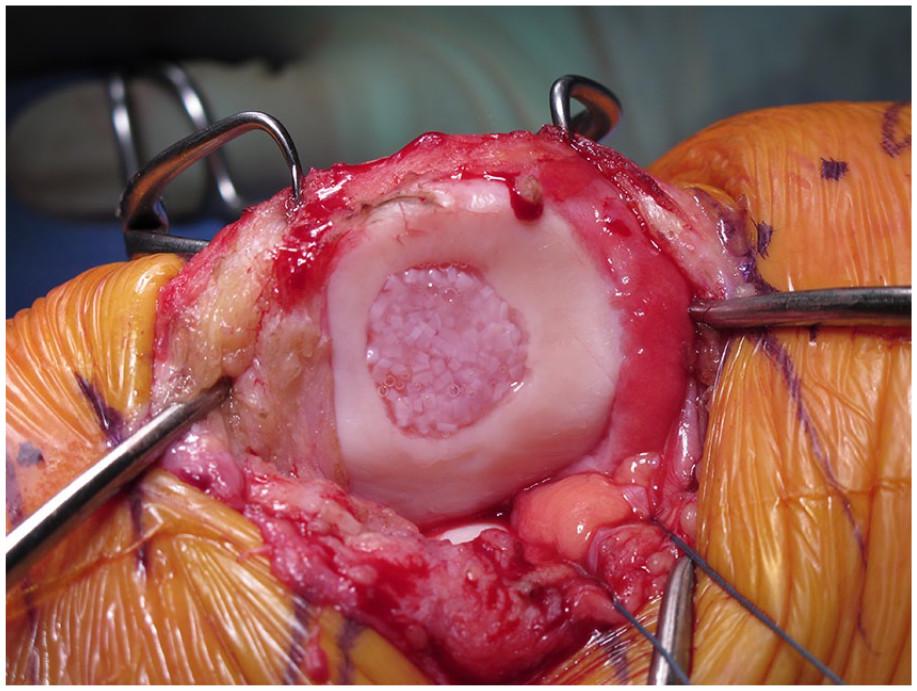
3 - Osteochondral graft -This is the most complex cartilage restoration operation and is usually indicated where there is considerable involvement of both the bone and overlying articular cartilage. Osteochondral graft involves removing a plug of bone and then using one’s own tissue or donor tissue to fill the defect. As above, there are pros and cons to each strategy.
Ready to take the next step?
Click on the 'GET IN TOUCH' button and provide your details,
and we'll reach out to arrange an appointment as soon as possible.
