Background
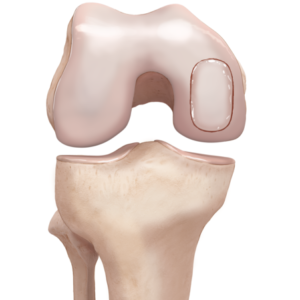
There are 2 main cartilage structures in the knee. The hyaline cartilage, also called articular cartilage, lines the end of the bone surfaces of the femur, tibia and patella (the kneecap), acting as a smooth, gliding surface permitting knee joint movement.
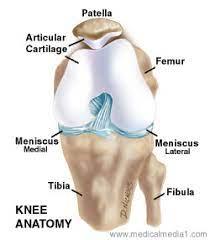
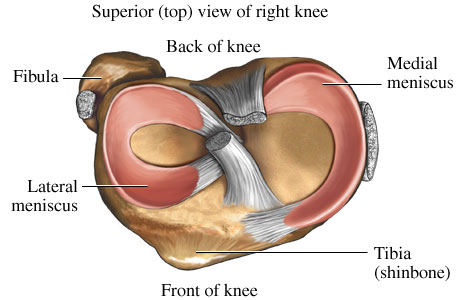
The meniscus, a second type of cartilage, acts as a shock absorber in the knee, preventing damage to the articular cartilage.
When articular cartilage is damaged, it often causes symptoms such as pain, swelling and locking in the knee. The cartilage relies on the surrounding joint fluid for its nutrition and has a poor blood supply, hence its inability to regenerate or heal on its own. If left untreated, damaged cartilage predisposes the knee to early arthritis.

Most of the time, damaged articular cartilage requires surgery to remove the non-healing tissue and then an additional procedure to restore or help to regenerate cartilage.
These procedures are described below:
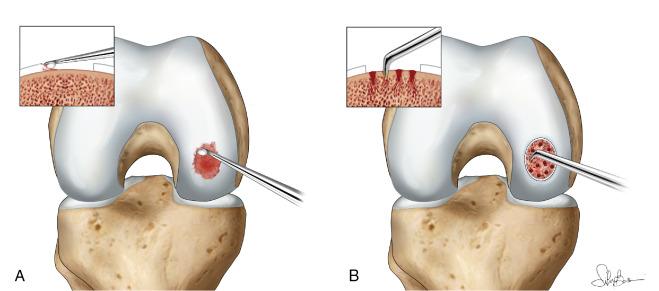
1 - Microfracture- this arthroscopic or ‘keyhole’ procedure involves making small perforations in the subchondral plate to cause bleeding and stem cells to migrate into the cartilage defect. ‘Scar’-cartilage or fibrocartilage is formed. This is not as robust as the native ‘hyaline’ cartilage
2 - Cartilage transplantation- cartilage can be harvested from the patient’s own knee in non-essential areas or can be obtained from a donor. There are pros and cons to each strategy. Harvesting one’s own cartilage can lead to ‘donor-site’ issues and is limited by the amount of non-essential cartilage available. For larger areas of damage, donor cartilage can be used to fill the defect. The donor cartilage is placed into the knee through an open procedure where the damaged tissue is removed and the donor cartilage is implanted. Donor cartilage carries the risk of allergic reaction, graft rejection by one’s own immune cells and infection.
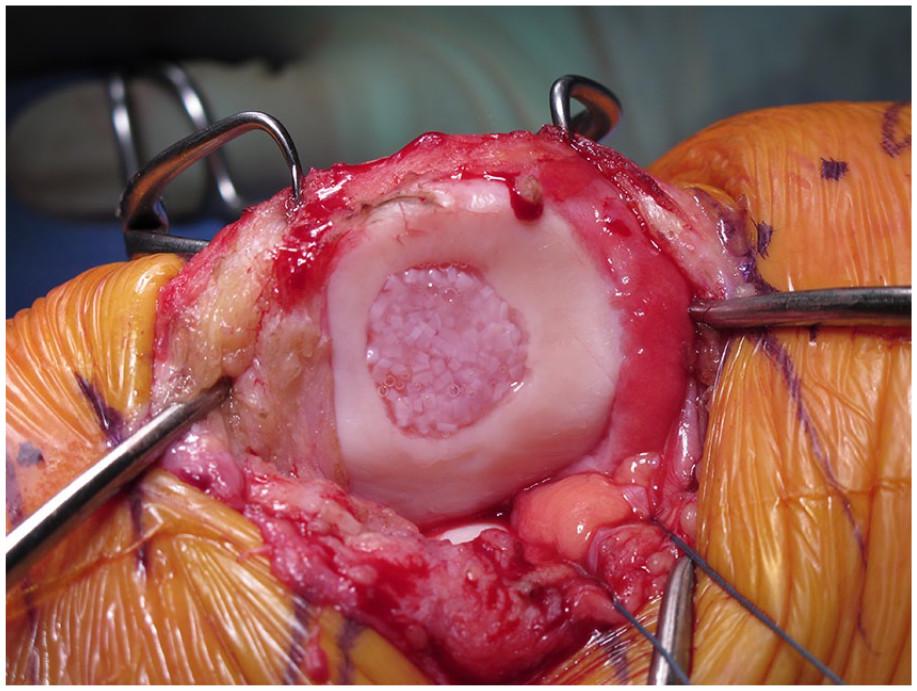
3 - Osteochondral graft -This is the most complex cartilage restoration operation and is usually indicated where there is considerable involvement of both the bone and overlying articular cartilage. Osteochondral graft involves removing a plug of bone and then using one’s own tissue or donor tissue to fill the defect. As above, there are pros and cons to each strategy.
| Phase | Goals | Weight Bearing/ROM Brace | Cardio/ROM | Strengthening |
|
Phase 1 Non Weight-Bearing Phase
(Weeks 0-6) |
|
NWB 6 weeks
|
Supine/seated ROM only
Heel Slides Heel Props Heel Hangs |
Multi Plane SLR
Multi Plane Hip Range IRQ Static quads, hamstrings, calf pumps |
|
Phase 2
Early Weight-Bearing (Weeks 6-8) |
|
|
Stationary Bike, no resistance to begin
Treadmill Walking |
**Body Weight Strengthening only
Flexion/Extension only, no side steps or side lunges Half squats, Ball squats Wall slides Bridges Forward lunges to 45° |
|
Phase 3
Strengthening (Week 8-16) |
|
WBAT |
Stationary Bike, no resistance to begin (wk 8-10)
Treadmill Walking |
Quads, hamstrings, calf strengthening
Hip abductor and adductor strengthening Step downs- front, back and lateral Lateral Lunges Romanian Deadlift unloaded from week 8, loaded week 10 From Week 12 Squats (to chair if appropriate) Single leg squats to 90° Loaded Squats and Deadlift from Single limb balance and proprioception |
|
Stage 4
Week 16+ Return to Sport |
|
WBAT |
Multi-plane plyometrics
Multi-plane Agility Cutting and Pivoting Exercises Ladder Drills Landing Mechanics |
Return to Sport Criteria
Single Leg hop Quads index > 95% Hamstrings index >95% Pain and swelling free post exercise |
This rehabilitation protocol relates to any cartilage restoration procedure performed by Dr. Cohen.
General Instructions:
Femoral Condyle and Tibial Lesions
Irrespective of the procedure, patients will remain Non-Weight Bearing (NWB) for 6 weeks
The knee will be placed in a Range of Motion Brace (ROM brace) permitting progressively increasing flexion angles.
- ROM 0-30° for 2 weeks
- ROM 0-60° weeks 2-4
- ROM 0-90° week 4-6
- Unlocked week 6-8
Patella and Trochlea Lesions
A ROM is to be applied 0-30° for 6 weeks when mobilising, Patient can weight bear as tolerated with crutches
The knee flexion angles will be allowed to progress slowly to prevent over loading of the PFJ
- ROM 0-30° for 2 weeks
- ROM 0-45° weeks 2-4
- ROM 0-60° week 4-6
- Unlocked week 6-8
No open chain exercises are allowed for 3 months following this procedure:
Ready to take the next step?
Click on the 'GET IN TOUCH' button and provide your details,
and we'll reach out to arrange an appointment as soon as possible.
